#21: How Will the Virtual Twin Transform MedTech?
Learn how virtual twin experiences are set to revolutionize medical device design, clinical trials and patient treatments.
#21: How Will the Virtual Twin Transform MedTech?
Virtual twin experiences and computational modeling and simulation are set to revolutionize device design, clinical trials and patient treatments. In this episode, we explore a compelling vision of how these advanced digital technologies can minimize risks, cut costs and expedite the product approval process. Click here to discover more about this topic.
This episode was recorded at Device Talks Boston in May 2024.

Meet our speakers


“Now, we can virtually place a device and look at how that changes the function, and maybe predict how the heart would remodel in response to getting that device.”
Ellen Roche
Read the transcript
Narrator: This is Disruptors Unleashed, the series that showcases the disruptive technologies — and the trailblazers — reshaping our world. Previously, we explored some of the new trends transforming the automotive industry, from the rise in electrification to the advent of software-defined vehicles.
Today, we look at how the virtual twin is changing the way medical devices are designed, manufactured and approved. Joining us are Ellen Roche, a professor at MIT, and Dr. David Hoganson, a pediatric cardiac surgeon at Boston Children’s Hospital.
Host, Tom Salemi: Hi, this is Tom Salemi of Device Talks, we're here on the floor of Device Talks Boston. Dassault Systèmes just delivered another great presentation about the digital twin. And we're going to actually have a conversation with two— they're two experts in the field who are on the panel, to better understand how this technology is really changing healthcare, changing product design. So, I'm here with David Hoganson. Dr. David Hoganson, you’re a pediatric surgeon at Boston Children's Hospital, and Ellen Roche of MIT. Very excited to have… both a return speaker and someone who I wanted to have as a speaker. And… she's here! So, it just, it just manifested itself, which is great. I'm really grateful to have this opportunity to talk to you about digital twin technology. We've had Dassault Systèmes at Device Talks Boston many times to talk about its potential. And it just— for me, it's great to hear how it's being applied in the field of healthcare and medical design.
Dr. David Hoganson: Yeah. So, you know, we're really excited with how we're being able to use modeling and simulation in pediatric cardiac surgery. And so, you know, certainly, the challenge is, you know, all of our patients are unique, and their congenital defects are unique. And what we need to do is to correct those, correct the anatomy and correct the physiology. And so, you know, often there's a fair bit of variability when you're doing the corrections just by visual estimation in the operating room. And so, our team is using 3D modeling of individual patients to plan the surgical reconstructions, and also using simulation in the means of flow simulation, so simulating the flow through the anatomy with these different surgical options, to try to better plan the right operation for these children.
Host: That's interesting. I always… not always, I would think that if someone says they have this defect, it's like repairing a car, like, “Oh, we'll just pull it out and put it in a new one.” But every— I'm sure every injury or every defect is different, and requires different sorts of services. Where does the information come from that's used in the creation of that digital twin, that allows for that modeling? Is that through pre-surgical imaging, is it other technologies?
Dr. David: Yeah, you know, certainly, I think… I think in the future, we're thinking about sort of, you know, models that affect an entire disease. But for us, it's very patient-specific, always. So, we do individual CT scans or MRIs of these patients, and then from that anatomy, that's where we create the model. So, it's always a model of their own individual defect. And then that's the substrate for all these engineering workflows to try to understand how do we do the repair more precisely and accurately. And then also, how do we make the best decision about what to do? Because sometimes it's not always clear, even from experience.
Host: That's interesting. Ellen— Ellen Roche, you're an MIT professor, you're involved in medical device design. How does the digital modeling play into what you're doing there?
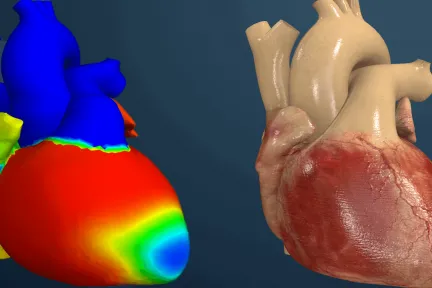
Ellen Roche: Yeah, thank you. We, um, my team at MIT, we use digital twins for most of our projects. So, we're interested in designing devices, you know, to either kind of locally repair or globally assist with... usually heart functions. And to do that in a better way, computationally, we can take a patient-specific model — again, not always pediatric, but you know, depending on what condition we're working on — and then we can actually simulate, you know, the function of that heart, for example, the structural motion of the heart and the flow inside the heart. And, now, we can virtually place a device and look at how that changes the function, and maybe predict how the heart would remodel in response to getting that device.
Host: How close is the model in terms of projecting the impact that this device is bringing?
Ellen: Yeah, exactly. Yeah, and, of course, we rely on clinical collaborators to get the data from the pre-procedural images. And then, if we can partner with them, and follow up to kind of validate that what we're predicting is actually what's happening. And I think we also, you know, rely a lot on building physical models to validate what we predict computationally.
Host: Interesting, how… and how accurate is the modeling? If it turns out one way on the virtual model, can you build it and be confident that it's going to do what it projected?
Ellen: That’s the hope. I mean, patients are variable, as Dr Hoganson mentioned, and responses kinda vary depending on who it is. But I think we can make a good prediction of how it would affect the mechanics of the system. And, you know, we can also, like I mentioned, build physical models to validate on a case-by-case basis that what we're predicting is actually what's happening. And I think it allows us to test a variety of designs and, you know, we can really be creative and you know, parameterize design aspects and then screen, you know, which aspect is most influential on the function of the device.
Host: So, let's do the forward-looking part of this conversation, where I pull up my big pipe and ponder the future. Where is this technology going to bring us, in your mind, and how close are we to that point? We'll answer part one of the question first: Where does virtual modeling fit into healthcare 10 years from now? David?
Dr. David: Yeah, I mean, I think from our standpoint, you know, what we've done is demonstrate that in individual patients and on a small scale, this can be very impactful, right? And so, you know, some of the workflows are used every single time we have, you know, one of those kinds of patients, and that's been remarkable. And what we're doing is now expanding these workflows to more defects, and more diseases and more issues, to achieve the same benefit for these other patients. So, I think it's really the vision is, you know, is how are we going to scale this? It's not a question of “Is it going to be helpful? Or is this going to allow us to do things better?” It's just a matter of how can we now efficiently do this for more patients, and, you know, we're using… we're using tools that are standard in other industries, but not really designed for this application. So, as this matures, you know, specifically tailoring these tools to allow us to do things quicker. And these other technologies, you know, the AI technologies and other things, which are going to really have an impact — maybe not today, but in the coming years — they're going to really make this a lot faster. So, we're excited about using all these different approaches to scale this, to reach more patients and more families who can really benefit.
Host: So, getting to that point, there's a 10-mile trip; what mile marker are we on right now?
Dr. David: I mean, some days, it feels like a few steps and some days, it feels like we're, you know, we're really rolling. So, you know, I think, as Ellen and I look at this, it's really about how do you do things in a super careful way so you build the trust of everybody, and then build on top of that. And so, you know, sometimes you have to, you know, start slow to run fast. And we're definitely, you know, the both of our teams are taking that same approach. And, and, you know, and once it's, it's, you know, really proven in each of these areas, then it's a matter of, you know, how do you then scale it quickly?
Host: And, Ellen, similar question in what you're doing with medical device design. Where are we headed? Where should we be in 10 years, with digital modeling? And… I guess, how would it— how do you see it sort of changing the whole process of medical design? I could see it being quite…
Ellen: Yeah, I think it has potential to make a big difference to the process. I think at every stage, there are tools that can really help to accelerate the process, right? In the early design prototyping stage, you can do that, or you work all the way through to testing and validation, maybe regulatory approval, and then even kind of predictive models and patient follow-up. So, I think there's multiple stages at which these tools can benefit the overall workflow. I think there are some challenges to adoption, like the time it takes, the expertise required, the infrastructure required to do it. But we're working to kind of, I guess, democratize it in some way and using these AI tools to make it faster, and, you know, build kind of data-driven models that are informed by these high-fidelity physical models. So, we can do it in a really, clinically practical time, you know, turn time.
Host: So, same 10-mile question: Where are we? Are we on the interstate yet or…?
Ellen: Yeah, maybe getting onto the interstate, I don’t know!
Host: So, we have a lot of progress to look forward to, what is going to— The final question, what's going to accelerate that? Is there something that's going to happen externally, either on the regulatory side or the insurer side, on the physician side, maybe new physicians coming in, same with new designers coming in who are more accustomed to this technology… Is there going to be a generational shift to people who are using this technology that's going to advance this? What's going to help us get further down that highway? David?
Dr. David: Yeah, I think everything you said, you know. It's a combination of a lot of things, I think some of it is adoption. And some of the things we're doing is the same operation, but just knowing which one to do. And those get adopted quickly. But when you're slightly shifting things, it just takes longer, right? And, you know, I think there's going to be, you know, new tools that are developed, and everything that we have is going to get quicker. And then as these young physicians come along, who've seen 3D models their whole career and their whole training, you know, they're going to want them for all of their patients. And, you know, I think it's going to take some time to spread from one institution to the other and then from one disease to the other. So, all these things take time, but I think it's just a matter of developing the tools and the processes that are trustworthy and really make a difference. And then the adoption will come.
Host: You know, same question to you, Ellen. I imagine your students coming in are going to be more and more and more and more comfortable with us, and it's gonna become the norm rather than the exception.
Ellen: Yeah, that’s the whole, I think… you know, this generation of students, they're so advanced at everything computational, but we really want them to be thinking of using these tools at every step of the way. And I think that's going to drive change. In addition to, I think if we can really address the credibility of these models in different fields, you know, in the design arena, in the clinical arena, in the regulatory arena, I think that will really help to accelerate it.
Host: Thanks, great. Well, it's exciting times and really happy to have Dassault Systèmes here at Device Talks Boston, kind of painting the future for us. So, we're grateful to have you both here with us in the studio to give us a little light on what's actually happening. Thanks so much.
Dr. David: Thank you. Thanks a lot.
Ellen: Thank you.
Narrator: Disruptors Unleashed is produced by Dassault Systèmes. For more episodes, follow us on Apple Podcasts, Spotify, Deezer, or your nearest streaming platforms. To learn more about Dassault Systèmes, visit us at 3ds.com.
Learn more

Virtual Twin Experiences for Sustainable Innovation – Helping People Live Healthier Lives