Enabling precision medicine
3D mockups have revolutionized how companies in aerospace, automotive and shipbuilding design, optimize and produce complex products. Now Dassault Systèmes is using virtual models to transform how the human body is understood, diagnosed, treated and cured. The goal: to create a holistic and integrative source of personal health information for patients and healthcare systems.
UNTIL NOW
Medicine was one-size-fits-all
FROM NOW ON
Virtual twins of the human body will enable precision medicine
Virtual twins of humans are the key to ushering in the next frontier in precision medicine. These experiential views of a patient’s unique anatomy and health status give practitioners an entirely new way to study each person, along with new methods of collaboration within the fragmented medical community. Moving from the traditional one-size-fits-all approach to one that treats each patient as an individual creates the possibility for better patient outcomes, through therapeutics tailored to target a specific disease for a specific patient, surgery and interventions designed to fit their unique anatomy and devices and prostheses engineered or printed on demand.
Extending its legacy of pioneering 3D virtual twin technology to transform the inorganic world, Dassault Systèmes is working on advanced projects in the organic world for the heart, brain and skin. Indeed, many therapeutic areas (cardiology, neurology, orthopedics, pulmonary) are already showcasing major innovations, with patients benefitting from unique and unprecedented treatments. Thanks to these first achievements, we are on the brink of producing a full virtual twin of the human body, making possible a holistic view of all facets of an individual’s health, fine-tuned by observations and measurements performed in the real world.
Toward a healthier future
Several initiatives are already helping researchers, device manufacturers and doctors to develop highly accurate virtual models for understanding disease, developing therapeutic solutions and assessing treatment options. Three of these projects, are well underway.
Modeling the human body is no longer a dream; it’s a commitment by Dassault Systèmes that will no doubt change the future of life for generations to come.
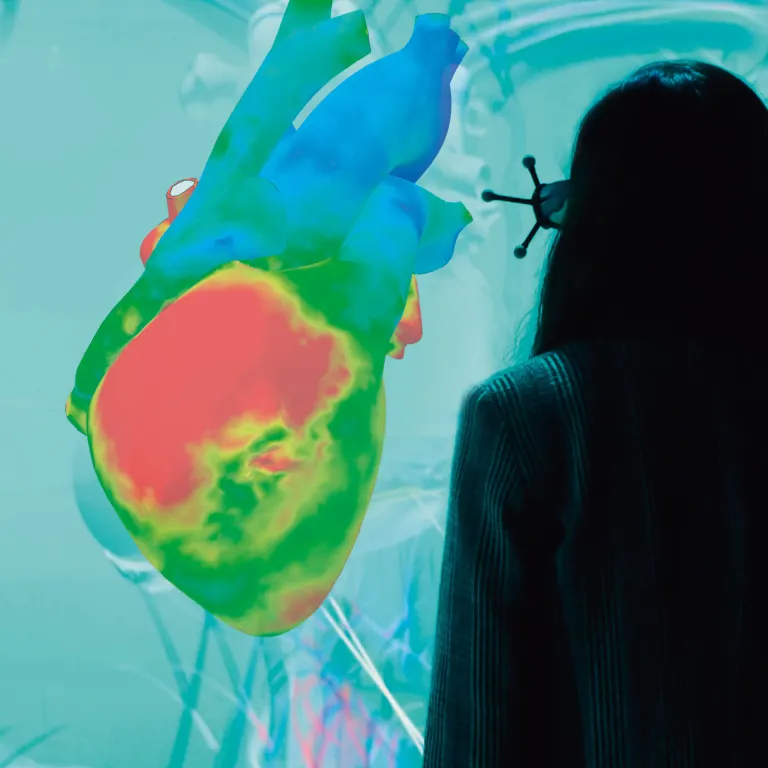
A 3D model of the complete human heart
The Living Heart Project (LHP), launched in 2014, brings together researchers, educators, medical device developers, regulatory agencies and practicing cardiologists to develop a scientifically accurate and fully functioning virtual model of the complete human heart – and apply it to improving outcomes for actual patients. The goal is to ensure the right approach is chosen for each person prior to surgery.
Constructed from an understanding of human heart tissue, structure and electrophysiology, and completely adaptable to mimic an individual person or a population, this virtual medical reference is in use around the world, helping to understand structural and hemodynamic heart disease.
Surgeons at Boston Children’s Hospital have used LHP technology to virtually plan surgeries, as well as to improve communication with the families of their young patients. Belgian digital health tech firm FEops has developed a virtual twin-based pre-operative planning platform for structural heart interventions. Researchers at McGill University, Montreal, used the model to understand the impact of COVID-19 on patients with heart conditions. And the US Food and Drug Administration (FDA) is leading a five-year project that will culminate in an in silico clinical trial using the 3D-simulated model to create a focus group of virtual patients. Experts believe the LHP has the potential to reduce human trials from years to days – a far more efficient method to achieve regulatory approval of cardiovascular medical devices while also reducing the burden on animal and human testing.
“I think there’s a lot of ways 3D models can impact how we treat tiny hearts with incredibly complex defects to really transform the patient experience.”
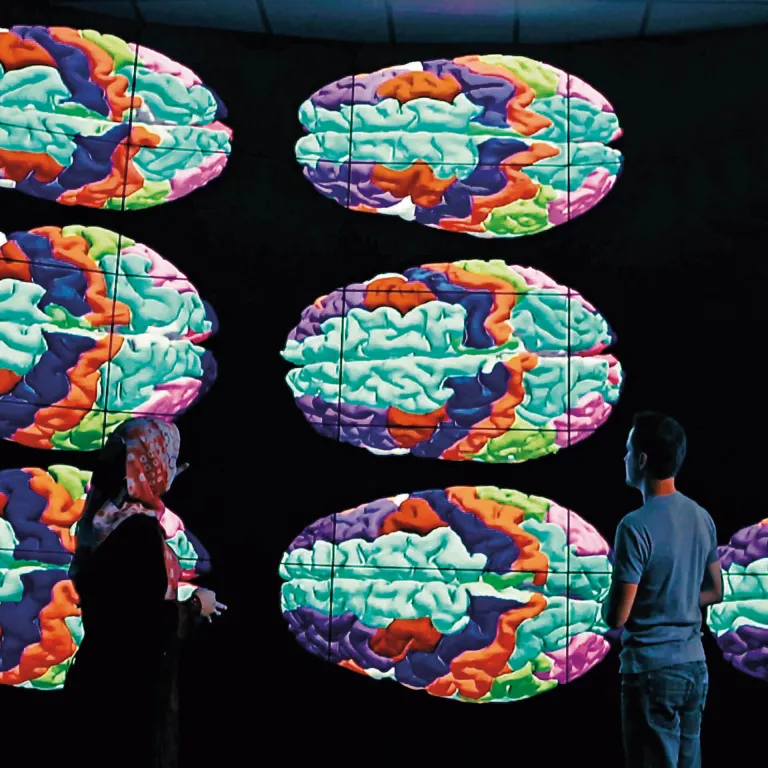
Modeling the brain in 3D
Discovering the success of the LHP prompted clinicians and neurologists to approach and get Dassault Systèmes involved in a project for help improving epilepsy surgery management and prognosis. The result: EPINOV, the Living Brain for epilepsy surgery project, a public-private partnership with French hospitals, especially the La Timone Hospital in Marseille (AP-HM), the Hospices Civils in Lyon (HCL), and the French Institute of Health and Medical Research (Inserm), under the lead of Aix-Marseille University (AMU).
A virtual twin of each patient’s brain holds great possibilities in epilepsy surgery, where the success rate is low for some kinds of epilepsies and errors in estimating the parts of the brain to target can result in cognitive deficits. Since 2018, a clinical trial has used virtual twins of the brain constructed from patient imaging and electrophysiological data calibrated to the typical seizures of a patient. This novel approach has the potential to raise the success rate of surgery for drug-resistant epilepsy patients.
“Using virtual twins for epilepsy surgery has the potential to significantly improve some people’s quality of life and reduce the burden for the system of care.”
Living skin: healing wounds
As the largest organ, skin provides many essential functions: from shielding against external aggressions by pathogens, chemicals and radiation to thermoregulation, and serving as the body’s alert system against harm. Dassault Systèmes has developed a multiscale model of skin, based on its fundamental molecular properties, that can accurately predict the penetration of chemicals through skin layers. This virtual model is being used to design predictable drug delivery systems for painless injections, secure wearables, and eventually, injectables that adapt to an individual’s shape, size, body chemistry and mobility.
Even more complex models of skin are being used to understand the dynamic process of wound healing, a major burden on the healthcare system.
But that’s just a start. In partnership with Urgo Medical and other experts, Dassault Systèmes has launched GENESIS, a project to create artificial skin for healing deep wounds, especially for burn victims. This represents an alternative to autografts, which require multiple surgeries, a long hospitalization and then ongoing treatment. The project also underlines the growing importance of virtual twins in advanced therapeutics for skin.
Accelerating precision medicine
Using regulatory grade, historical clinical trial data to augment or replace randomized controls, Medidata’s Synthetic Control Arm® (SCA), a type of external control, helps advance targeted therapeutics and personalized medicine. Awarded “Best AI-based Solution for Healthcare” in the 2021 AI Breakthrough Awards, Medidata’s SCA helps accelerate development of new drugs by combining virtual and clinical evidence, avoiding large randomized clinical trials. By merging personalized models with machine learning, the virtual twin will help sponsors develop drugs and patients get the best available treatment for them.
“We are convinced that by creating the virtual twin of the human body we can catalyze a transformation of the healthcare ecosystem and expand healthy expectancy within an efficient and sustainable healthcare system.”